A great advancement in health is that it’s become more mainstream for patients, their families and communities to be included in decisions about health.
What we haven’t been able to do as a sector is ensure that engagement is always meaningful, sustainable, and respects the time and energy that people give us.
So we need to reflect on why community engagement is needed and be clear about this.
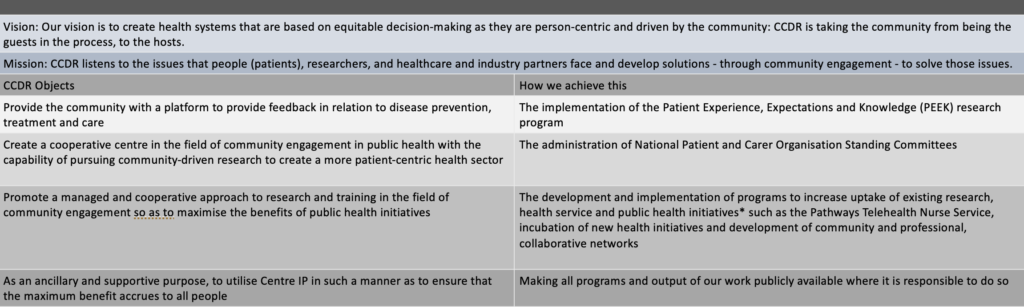
At CCDR, there are three reasons that we do what we do.

When we talk about infrastructure we often think of the physical structures and systems needed to deliver health services, basic research, clinical trials and so on. What we do not often talk about is the infrastructure needed to create an environment that supports community-based organisations to systematically collect patient experience data and implement health services. It is this kind of infrastructure that CCDR helps to create.
This is how we do it

Community engagement is often about giving up control. It means we enter conversations with an open mind and without a pre-determined outcome. This is why at CCDR we have:
PEEK as a platform for people to talk about their experience in the health system. The protocol is hypothesis generating which means we don’t enter the process with a pre-determined hypothesis. It’s systematic so that we reduce bias and remain independent.
NPON as platform to support patient organisations as professional bodies. CCDR act as a secretariat and use the feedback from patient groups to develop a program of work rather than a platform to drive a specific agenda.
Pathways as a platform for patients to access health services. The model of care allows for self-referral and focuses on empowerment for patients to be able to access the holistic care and management they need.


Personal Experience, Expectations and Knowledge (PEEK) studies use a single protocol. They are mixed methodology studies including an online questionnaire and structured interview. This approached is used as our aim is to have routine and proactive collection of patient experience and expectation data by an independent agency. All reports are publicly available and collectively, this results in a repository of patient experience data, with transparent and systematic presentation of results. The program is the result of 2 years protocol and feasibility testing. As at 2024, 2,000 patient interviews with matching data have been collected.
PEEK has a multi-dimensional protocol that can be cross-validated and covers a holistic range of domains. Participants in PEEK studies have the chance to reflect on everything they have experienced, then, acknowledging that they hold their own expertise, we ask them what their expectations and recommendations are for the future. This gives us all the direction we need to make decisions about treatment, care, information and communication.

In addition to the PEEK report, additional modules are possible to bring the patient experience to life. These include video interviews with patients and clinicians and patient groups; Clinical pathway reviews; Decision-maker briefs and ‘10 things you need to know’ flash cards.
CCDR has the capacity to conduct interviews in French, Spanish, German, Italian, Mandarin and Cantonese. Let us know if there are other languages that are important to your communities and we can arrange this.


Patient organisations are the heart and soul of the health system. They provide linkage between the patients and families that they support, and government, researchers, clinicians, service providers, policy-makers and industry. The National Patient Organisation Network (NPON) program provides a space for patient organisations that work at the grass-roots level, to come together – free from distraction – to develop solutions that work best for their patient populations, and represent their needs as a professional body. The NPON program is about developing practical solutions to health system challenges, actively designing systems and policies that work better for patients and their families, and leveraging the position of community-based organisations for health service delivery.
To really move forward and accept patient organisations as part of the health system and their important role informing decision about health, we have to consider the contribution they make, and this is a central aim of the NPON program
The first network was established in Australia as a pilot and you can get to know the community through the video below.
What’s next for NPON is to establish networks in as many countries as possible. This is an essential part of building the basic infrastructure needed for ongoing and routine community engagement in decisions about health and community-based service delivery. Once this kind of infrastructure is built, the network becomes a mechanism that can be leveraged for patient feedback, health service delivery, information dissemination and implementation of crisis/emergency support. We always make sure that engagement is done in a respectful way and so our approach is:



Pathways places specialist telehealth nurses in community organisations. It is a remote clinic that can be inclusive of families, carers, and patients. Pathways telehealth nurses are able to consult with patients living in all areas, including regional or remote areas, without any of these patients having to leave their home, or paying any costs associated with travel and accommodation to access health services. Most importantly, Pathways telehealth nurses help patients make the most of existing services within the health system. Pathways is also a community-based triage service that is being developing for more applications in in disaster and conflict settings. The care model remains nurse-led and covers out-of-hospital care. As an example, during the height of COVID when patients with chronic conditions weren’t able to access hospital care, nurses managed their care locally. As nurses ‘sit’ within community based organisations, they are well placed to keep patients out of urgent care where possible, and when they do need urgent care, pick up their care following discharge to ensure discharge plans are following with continuity of care and rehabilitation.
For community-based organisations, Pathways means that they don’t have to have their own infrastructure, training, clinical guidance and monitoring and so on in order to have a specialist nurse for their community. CCDR provides the core infrastructure so that even the smallest of patient groups can have their own Pathways nurse.

The Liberal National Government is providing more than $1.5 million for a new pilot program that will help patients of serious and rare diseases connect with the best health services and treatment.
The funding over three years will be provided to the International Centre for Community-Driven Research to deliver the Patient Pathways Program.
This program will help those diagnosed with certain, often rare diseases better navigate the health system and will also inform future research and expanded support for patients.
The Patient Pathways program will commence in 2019 with the inaugural Patient Organisation Annual Conference scheduled for May 2019.

Initial funding for the Patient program was provided through the Australian Department of Health in 2019. This was following a meeting with the Hon Greg Hunt MP, then minister for health. Minister Hunt invited CCDR to prepare a proposal to address issues of health system navigation that patients were facing. CCDR had been implementing a health system navigation service and the basis of the proposal was to test the protocol in a number of disease areas.
Funding was provided to CCDR and distributed amongst patient organisations. Funding for this Pilot ended in June 2022.
WHAT WE HAVE NOW THAT WE DIDN’T HAVE BEFORE THE PATHWAYS PILOT
Nurse-led interventions were confirmed in the pilot so we are clear on what’s possible in a community-based, nurse-led Telehealth clinic:
* Initial assessment * Diagnosis assessment * Symptoms and comorbidities assessment * Information assessment * Symptom tracking * Health literacy assessment * Nurse education session referral * Record family history * Primary care assessment * MDT assessment * Clinical trial assessment * Point of coordination assessment * Emotional and social assessment * Distress/anxiety tool * Pain assessment * Palliative care assessment * Advance care planning * Surgical and hospitalisation history * Current and planned medications * Urgent care prevention + continuity of care on discharge from urgent care
CLINICAL GUIDELINES FOR NURSE-LED TELEHEALTH CLINICS
CLINICAL PROTOCOLS
TRAINING MODULES + PEER SUPPORT + CLINICAL MONITORING
CENTRAL INFRASTRUCTURE = COST SAVINGS
TIME REQUIRED PER PATIENT WAS ANALYSED = MORE ACCURATE RESOURCE PLANNING
Pathways can be adapted for uptake any country
Get in touch if your patient organisation or community you support needs a Pathways service


Australian Primary Care Nurses Association President’s Award 2024
The Australian Primary Care Nurses Association President’s Award, is only given occasionally to nurses that leave a lasting legacy in the primary health care system. Kate Holliday received this award in 2024 for the lasting legacy of the work implemented through CCDR and Pathways. APNA considered Kate’s work to be exemplary and a strong example for all nurses as to what is possible when a nurse looks at how great care can be provided to their community.
- The combining of disciplines including nursing, nutrition, health promotion and health science to create powerful impacts in your work.
- Research into the relationship between clinical research and its translation into policy, clinical practice and population health.
- The reach of work including with government, industry, not-for-profits, NGOs and research organization at a local, national and international level.
- The impact of work which, among many achievements, also includes the development of the Pathways Telehealth Nurse Specialists program. The element of capacity building in this program was particularly noted by the APNA Board.
2019 – 2020
2020 – 2021
2021- 2022
2022 – 2023
• 3060 patients accessed the program between August 2019 and June 2022.
• Overall there were 26,953 referrals, assessments or interventions made at an average of 8.81 per patient.
• Number and type of services and opportunities accessed included: 1669 Multidisciplinary team assessment; 2261 Primary care assessment; 1861 Pain assessment; 1916 Palliative care assessment; 1988 Clinical trials assessment; 2323 Home status assessment; 2072 Symptom management assessment; 9407 Information & education provision; 3456 Allied health and supportive care referrals
• Nurses are most commonly speaking with women (65.98%)
• Across all age groups, the highest number of people accessing the service were under the age of 18 along with a parent or next of kin (n=435, 14.22%).
• The service was designed to take advantage of the close relationship patient groups have with the community. The majority of patients found the service through their local patient organisation website or Facebook page (n=1474, 48.17%).
• Pathways Telehealth Nurses provided services across 9 broad disease areas. The most common conditions were diseases of the nervous system (n=1254, 40.98%). After this, developmental abnormalities (n=377, 12.32%), diseases of the digestive system (n=309, 10.10%), endocrine, nutritional or metabolic diseases (322, 10.52%) and mental, behavioural and neurodevelopmental disorders (n=318, 10.39%), and rare cancers
(n=355, 11.60%), all had between 300 and 400 patients accessing the service
• A cost analysis is available in the 2020 report and this has been validate in the 2021 report. In the 2020 review we reported that there was an average cost per patient of $65.84. This was confirmed in the 2021 report where the cost per patient was only slightly higher across both years at $67.37. The increase is because in the first evaluation, nurses spent less time per patient (1.58 hours) compared to 1.61 hours in the most recent report.
• The prgram was funded for 10 partner organisations to be involved. Over the life of the program, 18 disease areas were serviced through the grant.
• For the first time, we have guidelines to support nurses working in health charities, a basis on which to cost human resource needs, and a scope of practice for Patient Pathways Telehealth Nurses.
• Dr Kate Holliday who developed the Patient Pathways program has been recognised by the World Health Organisation, International Council of Nurses, United Nations Population Fund and Women in Global Health as a finalist for the 100 outstanding nurse and midwife leaders in 2020. In 2022 she was one of only three finalists for the 2022 Health Minister’s Award for Nursing Trailblazers in recognition of the Pathways Telehealth Nurse program.
• The Pathways Telehealth Nurse and NPON models are now in development for uptake in a number of countries


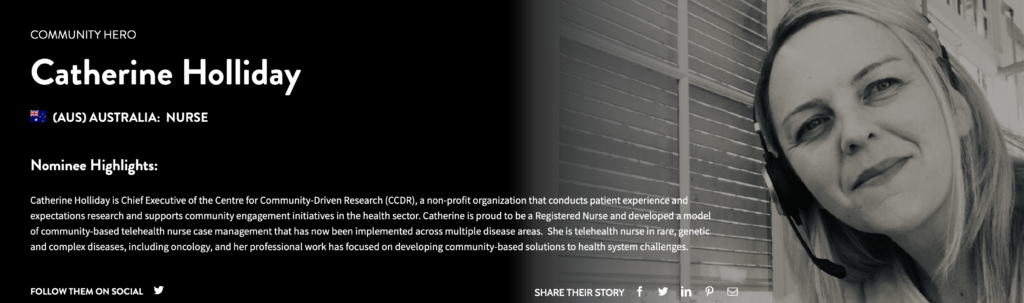
CCDR is led by Kate Holliday who is a nurse and researcher. Her education includes a Bachelor of Nursing degree, a graduate diploma in nutrition, a Masters in Health Promotion, a Masters in Health Science and her PhD thesis investigates the relationship between research and how to translate results into policy, clinical practice and population health. She has worked in the health sector for more than 20 years. In 2020, Kate was listed on the 100+ Outstanding Women Nurse and Midwife Leaders by Women in Global Health, World Health Organisation and partners, in 2022 became an alumna of the prestigious Australian Health Minister’s Award for Nursing Trailblazers and in 2024 was awarded the APNA president’s award for a legacy contribution to primary health care.
Her clinical work has focused on community-based case management and health system navigation, most recently in rare, genetic and complex conditions, and she has worked as a nurse in Australia and the USA. Kate developed and tested a model of community-based nursing care that in 2019 was expanded into a pilot program across 10 disease areas. This is through the Patient Pathways program funded by the Australian Federal Department of Health.
Kate has significant experience working with government, industry, not- for-profit organisations as well as research and international organisations including working in Geneva, Switzerland with the GAVI Alliance and Australian Department of Foreign Affairs and Trade (Health and human rights portfolio). She has also worked in leadership roles including Head of Research at Cancer Council and Head of Policy and Strategy at the Kinghorn Cancer Centre. Kate served as a Board Director at Health Technology Assessment International (HTAi) and Chief Executive at the Centre for Community-Driven Research. Kate is also the only nurse representative in the WHO Global Alliance for Care of the Injured (GACI) member leads the advocacy and allied health integration stream.
CHIEF EXECUTIVE MESSAGE
There is a story behind every treatment, health policy, and clinical protocol breakthrough that we have today. The story begins with a patient and an unanswered question, an observation leading to research, and a discovery that is translated into clinical practice.
There are however many unanswered questions that research is yet to answer. For too many patients, treatment options are either not available or not accessible; but we will never find the answers if we aren’t asking the right questions. To give us the best chance of providing patients with timely access to treatments and health services, we need to ensure that we, as a sector, are listening to the issues that patients are facing and clinical trends, to give us clues and direction for research, treatment and health service development. The Centre For Community-Driven Research provides a platform for this to happen, for patients and their families to be heard.
It has been a great honour to provide a closer connection between the research and health industries and the communities that they aim to benefit. At CCDR, our definition of community includes patients, carers, clinicians, researchers, policy makers, industry, and all stakeholders that have a role to play in improving our health system and advancing medical research. It is less about ‘us and them’ and more about what we can do as a community that values the experience of patients and their families, the expertise of clinicians and researchers, and the contribution of industry.
Ultimately however, we need to change the paradigm from patients being guests in the decision-making system, to the hosts.
We are proud to be able to provide a place for people and organisations to connect and learn from each other. However, we can not do any of this work without patients and families that give their time to share their experience with us, and to those people we sincerely thank you.

Alignment with constitution